(Tom: I am reproducing the article in its entirety so if the link gets broken you still have the data. To add to the recommendations of the good doctor I would add thet it has been found advisable to take vitamin K2 with the D3 to prevent hardening of the arteries by the D3.)
Throughout his career Dr. Eisenstein looked for way to protect his patients from infection and chronic illness. For the last years of his life his first in line prescription was consistently the same Vitamin D and Probiotics. Below are his recommendations.
Vitamin D Recommendations
1. Adult (and children ........................... 5,000-10,000 IU daily.
2. Children's maintenance: <100lbs.......... 1,000IU/25lbs. daily.
3. At the first symptoms of a cold or flu
1,000IU/ lb. daily for 7-14 days.Examples:
50 lbs. daily……….50,000IU daily.
100 lbs. daily………100,000IU daily.
Probiotic Recommendations CFU (Colony Forming Units)
Adults………………………. 20 billion CFU per day
Children………………. 5 billion CFU per daily
At the first symptoms of a cold or flu
Adults……………………… 50 billion CFU per day 7-14 days
Children…………………………….. 20 Billion CFU per day 7-14 days
By Danish Hameed
When new virulent diseases emerge, such as SARS and Covid-19, scientists and labs begin to find new vaccines and treatments for those affected. As the current crisis unfolds, governments are enforcing quarantine and isolation and public gatherings are being discouraged. Health officials took the same approach 100 years ago, when influenza was spreading around the world. Though the results were mixed, records from the 1918 pandemic suggest that a few things proved quite helpful while dealing with influenza. Some hard-won experience from the greatest pandemic in recorded history could help us in the weeks and months ahead in view of the COVID 19.
In 1918, it was recorded that severely ill flu patients nursed outdoors recovered better than those treated indoors. A combination of fresh air and sunlight seems to have prevented deaths among patients and infections among medical staff. There is scientific support for this and research show that outdoor air is a natural disinfectant. Fresh air can kill the flu virus and other harmful germs. Equally, sunlight is germicidal and there is now evidence that it can kill the flu virus as well.
‘Open-Air’ Treatment in 1918
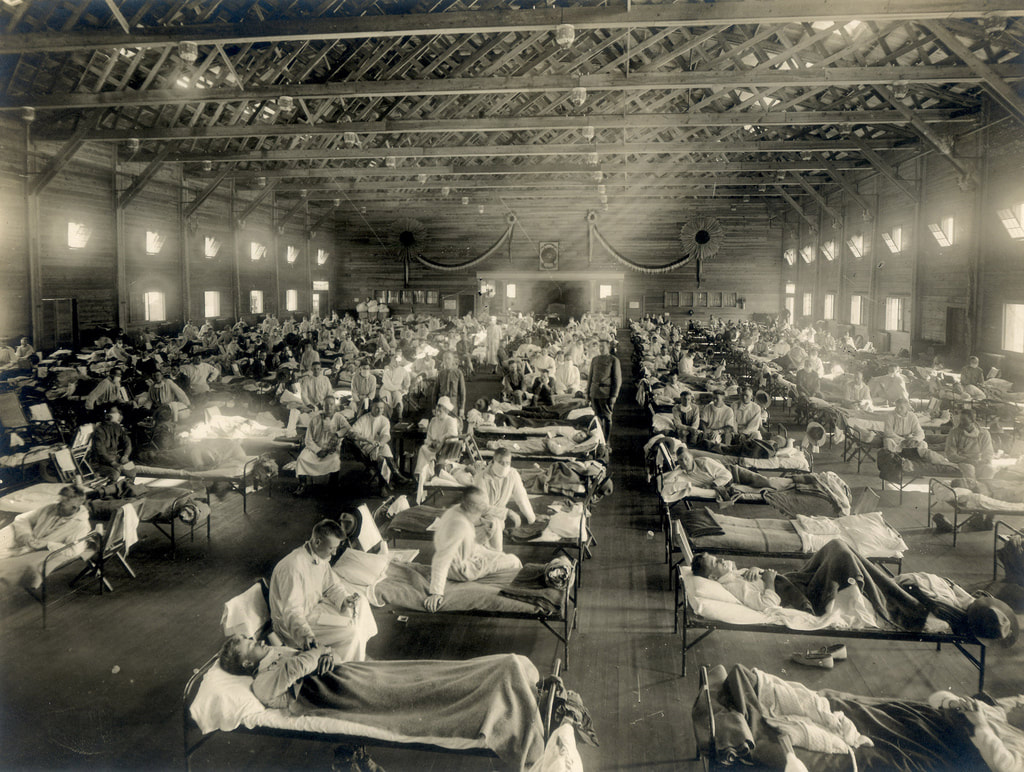
During the great pandemic, two of the worst places were military barracks and troop-ships. Overcrowding and bad ventilation put soldiers and sailors at high risk of catching influenza and the other infections that often followed it. As with the current Covid-19 outbreak, most of the victims of so-called `Spanish flu’ did not die from influenza: they died of pneumonia and other complications.
When the influenza pandemic reached the East coast of the United States in 1918, the city of Boston was particularly badly hit. So the State Guard set up an emergency hospital. They took in the worst cases among sailors on ships in Boston harbour. The hospital’s medical officer had noticed the most seriously ill sailors had been in badly-ventilated spaces. So he gave them as much fresh air as possible by putting them in tents. And in good weather they were taken out of their tents and put in the sun. At that time, it was a common practice to keep sick soldiers outdoors.
Open-air therapy, as it was known, was widely brought into use when dealing with patients from the Western Front. And it became the treatment of choice for another common and often deadly respiratory infection of the time; tuberculosis. Patients were put outside in their beds to breathe fresh outdoor air. Or they were nursed in cross-ventilated wards with the windows open day and night. The open-air regimen remained popular until antibiotics replaced it in 1950s.
Doctors who had first-hand experience of open-air therapy at the hospital in Boston were convinced that the regimen was effective and the same technique was adopted elsewhere. If one report, that was published in this regard, is correct, the treatment reduced deaths among hospital patients from 40 per cent to about 13 per cent. According to the Surgeon General of the Massachusetts State Guard: “`The efficacy of open air treatment has been absolutely proven, and one has only to try it to discover its value.”
Fresh Air is a Disinfectant
Patients treated outdoors were less likely to be exposed to the infectious germs that are often present in conventional hospital wards. They were breathing clean air in what must have been a largely sterile environment. We know this because, in the 1960s, Ministry of Defence scientists proved that fresh air is a natural disinfectant. Something in it, which they called the Open Air Factor, is far more harmful to airborne bacteria — and the influenza virus — than indoor air. They couldn’t identify exactly what the Open Air Factor is. But they found it was effective both at night and during the daytime.
Their research also revealed that the Open Air Factor’s disinfecting powers can be preserved in enclosures — if ventilation rates are kept high enough. Significantly, the rates they identified are the same ones that cross-ventilated hospital wards, with high ceilings and big windows, were designed for. But by the time the scientists made their discoveries, antibiotic therapy had replaced open-air treatment. Since then the germicidal effects of fresh air have not featured in infection control, or hospital design. Yet harmful bacteria have become increasingly resistant to antibiotics.
Sunlight and Influenza Infection
Putting infected patients out in the sun may have helped because it inactivates the influenza virus. It also kills bacteria that cause lung and other infections in hospitals. During the First World War, military surgeons routinely used sunlight to heal infected wounds. They knew it was a disinfectant. What they didn’t know is that one advantage of placing patients outside in the sun is that they can synthesise vitamin D in their skin if sunlight is strong enough. This was not discovered until the 1920s. Low vitamin D levels are now linked to respiratory infections and may increase susceptibility to influenza. Also, our body’s biological rhythms appear to influence how we resist infections. New researches suggest that they can alter our inflammatory response to the flu virus. As with vitamin D, at the time of the 1918 pandemic, the important part played by sunlight in synchronizing these rhythms was not known.
Image source: https://thekashmirimages.com/2020/03/16/a-lesson-from-the-1918-influenza-pandemic/
Article source: https://www.prod5.com/a-lesson-from-the-1918-influenza-pandemic.html
