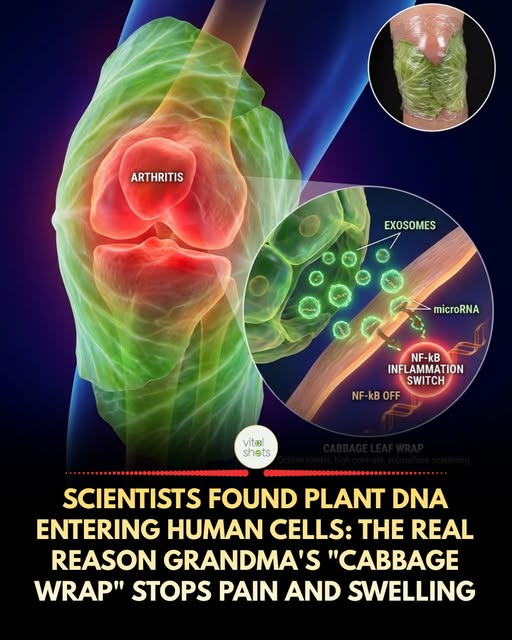
For centuries, breastfeeding mothers and arthritis patients have used Cabbage Leaves to reduce swelling. Doctors dismissed it as a “placebo” or just a “cooling effect.” They were wrong.

Tom's Blog on Life and Livingness
For centuries, breastfeeding mothers and arthritis patients have used Cabbage Leaves to reduce swelling. Doctors dismissed it as a “placebo” or just a “cooling effect.” They were wrong.
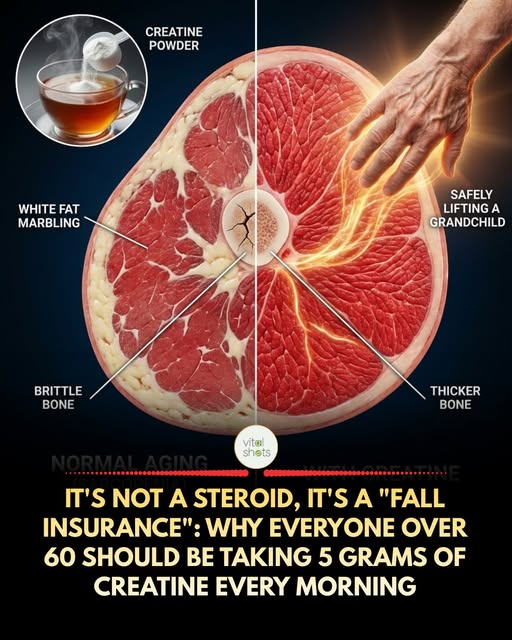

Raw, whole garlic does not contain Alicin (the magical anticancer and antibiotic compound). Garlic contains two separate ingredients: Aliina (protein) and Alinase (enzyme). They are in separate compartments. Only when you crush or grind garlic, you break cellular walls and allow the two to mix. They need to react chemically to create the Alicina. This reaction takes a while. And more importantly: Alinasa enzyme dies of heat.
The Common Mistake: You chop garlic and throw it in hot oil in 30 seconds. Heat kills the enzyme before it had time to create the Alicina. You eat delicious garlic, but medically useless.
Hack Tip to Vitalize Garlic:
Chop or crush the garlic, leave it on the cutting board then wait 10 minutes. During this time, the reaction occurs and the maximum amount of Alicina is created. Once created, Alicina is heat resistant.
Now you can cook it. This simple step of patience turns your dinner into a preventative chemo session.
Source: Journal of Nutrition, “The influence of heating on the anticancer properties of garlic”, Biochemistry Study.
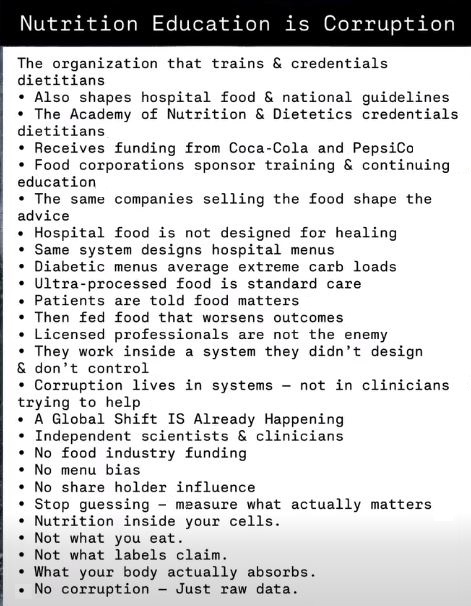
My observation is that this institutional bias is a common paradigm working to preserve the status quo and not alienating corporate sponsors. It takes a disappointingly remarkable level of integrity to stand against the corruption.
You may have heard the old saying, “He who has the gold rules.”
In order to achieve the best results for you and yours you need to listen less to self-proclaimed experts and authorities and look to see what is actually there.

You’ve been there. After a period of indulgence in ultra-processed convenience foods, fast food, or sugary treats, your body signals its distress with fatigue, bloating, mental fog, or inflammation. Modern industrial diets are an assault, deliberately overloaded with toxic pesticides, genetically modified ingredients (GMOs), artificial additives, and inflammatory seed oils. [1][2] These substances challenge our liver, kidneys, and digestive system, creating a toxic burden that corporate food systems and pharmaceutical giants are all too happy to exploit.
Yet, here is the liberating truth: your body is not broken. It is a masterpiece of biological intelligence, designed for resilience and self-repair. Moving forward is not about guilt or subscribing to another punishing fad. It is about empowering your body’s innate healing systems with the right, clean tools. This natural reset is a testament to the body’s inherent wisdom—a philosophy worlds apart from the symptom-suppressing, dependency-creating mindset of Big Pharma and the processed food industry. It’s time to reclaim your health sovereignty.
Keep reading: https://food.news/2026-02-01-how-to-reset-your-body-after-unhealthy-eating.html
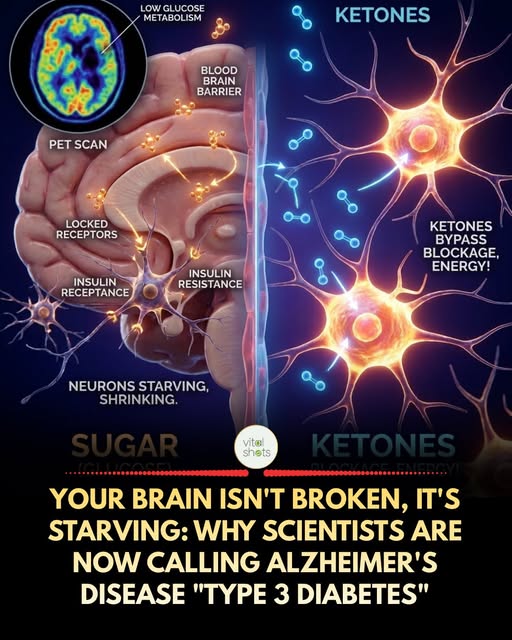
For decades, we thought Alzheimer’s was just “bad luck” or “amyloid plaques.” Now, a growing body of evidence suggests it is primarily a Metabolic Disease.
Just like your muscles can become insulin resistant (Type 2 Diabetes), your brain can become insulin resistant. When this happens, neurons can no longer absorb Glucose efficiently. Even if your blood sugar is high, your brain cells are starving to death. This starvation leads to cognitive decline, memory loss, and eventually, the death of the tissue.
The “Hybrid Engine” Solution
If the “Gasoline” (Glucose) line is clogged, you can switch to the backup fuel: Ketones. Ketones (produced during fasting or a high-fat diet) do not require insulin to enter the brain. They cross the blood-brain barrier and feed the starving neurons directly.
Studies show that when Alzheimer’s patients are given MCT Oil or a Ketogenic diet, their cognitive scores often improve because the lights turn back on.
Vital Advice
The Brain Fuel Swap: You don’t have to be fully Keto, but you must protect your brain’s insulin sensitivity.
Cut Liquid Sugar: Soda and juice are neurotoxins.
MCT Oil (C8): It converts directly into ketones in the liver, providing instant brain fuel even if you eat carbs.
Exercise: It restores insulin sensitivity in the brain.
Source: Journal of Alzheimer’s Disease, “Brain Energy Metabolism, Glucose, and Ketones”, Type 3 Diabetes Hypothesis.
(Tom: A great many plants have properties that help regulate blood sugar. So much so that I recall reading of two separate researchers who reported people eating raw food for 30 days lost their classification as diabetics.)
In 1993, during the filming of “Tombstone”, Val Kilmer was fighting a high fever while delivering lines that would define his career. Playing Doc Holliday, a dying Southern gambler with a deadly aim and sharper wit, Kilmer transformed what could have been a supporting character into the film’s most magnetic force. Under layers of pale makeup and labored breath, he delivered each line with a precision that blended elegance and fatalism. The phrase “I’m your huckleberry,” coolly spoken before a gunfight, became a signature moment that still echoes through pop culture.
Kilmer had immersed himself in research before the cameras rolled. He read deeply about John Henry “Doc” Holliday, a former dentist from Georgia who had tuberculosis and lived most of his final years gambling and gunfighting. Kilmer brought the illness to life without exaggeration. He adjusted his breathing pattern to sound like Holliday was constantly on the edge of collapse. He held ice cubes in his hand between takes to simulate clammy fingers. He even requested his character’s dialogue be trimmed into slower, drawn-out Southern rhythms. Director George P. Cosmatos later admitted that Kilmer came prepared with a full vision of Holliday that the crew had not anticipated.
The script for “Tombstone” (1993) gave Holliday a number of sharp quips, but it was Kilmer’s delivery that gave them staying power. When he tells Johnny Ringo, “You’re no daisy at all,” it is not mockery but something closer to pity. He plays Doc like a man already halfway to the grave, smiling at the chaos around him. While Kurt Russell commanded as Wyatt Earp, Kilmer floated through scenes with eerie grace, like death itself wearing a silk vest.
Off screen, Kilmer kept to himself. He did not break character often, preferring to stay in Holliday’s world even during breaks. Michael Biehn, who played Ringo, later said Kilmer’s focus unnerved him at times because it felt like he truly believed in the character’s fatal edge. That commitment didn’t go unnoticed. Russell, who also helped shape much of the film behind the scenes, later said Kilmer’s portrayal gave “Tombstone” its emotional backbone. His performance grounded the violence in something personal, something painful.
One scene stands above the rest. Near the end of the film, Doc lays dying in a Colorado sanitarium. Earp visits him for the final time. Doc looks down at his feet and softly says, “I’ll be damned. This is funny.” Kilmer’s delivery turns that line into a quiet acceptance of death. There are no tears, no declarations. It is a man meeting his fate with dignity and a bitter smile. The scene is haunting because of its restraint. Kilmer didn’t ask for sympathy. He earned it through silence and control.<
Even thirty years later, Kilmer’s work in “Tombstone” is regularly cited as one of the greatest performances in a Western. Fans continue to quote his lines at screenings. Memes and T-shirts carry his phrases. But more than anything, what remains is the image of Doc Holliday sweating through his linen suit, coughing into a handkerchief, and stepping into one last duel with the line that no one can forget.
Kilmer’s Doc wasn’t about guns or bravado. He was about loyalty, decay, charm, and pain stitched into one unforgettable presence. That kind of role doesn’t happen often. That kind of performance, even less.
His whisper of “I’m your huckleberry” still sends a chill through every saloon door memory and late-night rewatch. Every time the line plays, Kilmer lives again in smoke and silver.
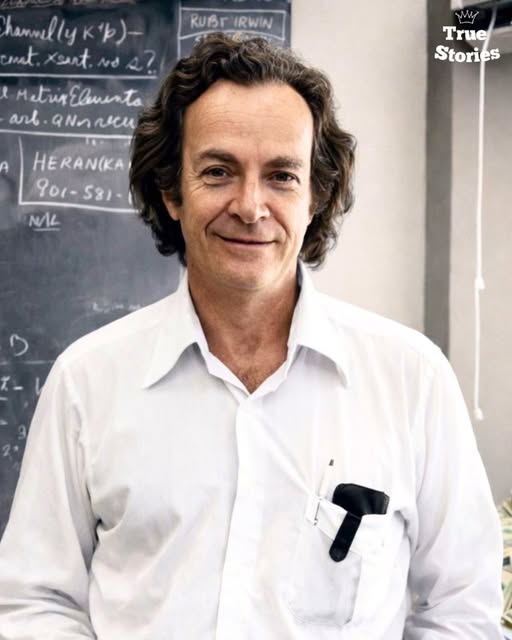
Richard Feynman embarrassed NASA on live television and forced the country to watch how easily intelligence gets buried by
procedure.
In 1986, after the Space Shuttle Challenger exploded, Feynman was appointed to the Rogers Commission as a symbolic gesture. A Nobel Prize physicist added for credibility. NASA assumed he would sit quietly while engineers handled the narrative. They miscalculated.
Inside closed sessions, Feynman discovered something worse than a technical failure. Engineers had warned management for years that the O-rings failed in cold temperatures. Data existed. Memos existed. Launches continued anyway. Risk had been normalized through language, not science (Rogers Commission Report; NASA internal memoranda).
Feynman refused the script.
At a televised hearing, he took a small clamp, a piece of rubber, and a glass of ice water. He submerged the O-ring material, removed it, and showed that it no longer returned to shape. No equations. No abstractions. Just physics. The room went quiet. NASA’s explanations collapsed in under thirty seconds (C-SPAN archival footage).
By the third turn, the consequence was institutional exposure. Feynman bypassed management entirely and published his own appendix to the final report, directly contradicting NASA leadership. He wrote that NASA’s stated risk estimates were fantasy and that reality was being replaced by wishful thinking. His line cut deeper than the demonstration. “For a successful technology, reality must take precedence over public relations, for nature cannot be fooled” (Rogers Commission Appendix F).
NASA was furious.
Internally, Feynman was treated as disruptive. He ignored hierarchy. He spoke directly to engineers instead of executives. He refused to soften language. The system could tolerate failure. It could not tolerate being exposed as dishonest. After the report, NASA adopted safety reforms without acknowledging how aggressively it had resisted them (NASA post-Challenger reviews).
This is the part the legend avoids.
Feynman did not save NASA. He outed it. He showed that catastrophic failure was not caused by ignorance, but by obedience. Smart people had been trained to defer to process over evidence. The explosion was not an accident. It was an outcome.
Feynman knew what it cost him. He was already dying of cancer. He had nothing left to trade for access. That made him dangerous. He told the truth because there was no future leverage to protect.
The cold truth is this. Richard Feynman did not expose Challenger because he was brilliant. He exposed it because he refused to play along. Intelligence is common. Honesty under pressure is rare. Systems do not fear failure. They fear someone who makes failure undeniable.
Sources (in text):
– Rogers Commission Report on the Space Shuttle Challenger Accident (1986)