This is an extract from a post advertisement I saw on Facebook.
I’ve been a legal drug dealer for nearly a decade, yet nobody believes me when I tell them these things.
When I say “legal drug dealer,” I mean I’ve been in the supplement and wellness industry for almost 10 years, watching people spend thousands of dollars on metabolism boosters and energy supplements, treating symptoms instead of addressing what’s actually breaking down inside their cells.
And the truth is, most people are walking around with severe mitochondrial dysfunction without even knowing it.
And it’s not your fault.
By age 40, your mitochondrial function declines by up to 50%. These cellular powerhouses that produce 90% of your body’s energy start failing. They can’t generate ATP efficiently, can’t support your metabolic rate, and just slowly shut down your cellular energy production.
So what do you do?
If you’re tired, you drink coffee. Your metabolism feels sluggish, you take fat burners. Energy drops, you try Adderall or Modafinil. Brain feels foggy, you add Alpha Brain or Lion’s Mane. Can’t focus, you stack more stimulants. You feel cold all the time, you layer up.
But here’s what nobody tells you…
When your mitochondria stop producing energy efficiently, everything slows down:
Your metabolic rate drops because cells can’t burn fuel properly.
Brain fog sets in because your brain uses 20% of your body’s energy.
You feel cold because mitochondria generate 85% of your body heat.
Mental fatigue hits because neurons need massive amounts of ATP.
This is the connection nobody talks about: slow metabolism and brain fog aren’t separate problems. They’re both symptoms of the same cellular energy crisis happening in your mitochondria.
Most people are taking 5, 6, even 10 different metabolism boosters and nootropics every day, spending $300+ per month on their stack, and still feeling exhausted, mentally foggy, cold, and watching their metabolism slow down year after year.
Why?
Because they’re treating individual symptoms instead of fixing the root cellular energy crisis happening inside your mitochondria—the metabolic powerhouses at the cellular level that are supposed to keep your body running at peak capacity.
I’ve seen this pattern with thousands of patients over the years.
They come to me with cabinets full of expensive supplements, frustrated that they’re still dealing with crushing fatigue, persistent brain fog, feeling cold constantly, sluggish metabolism, and this creeping sense that their entire system has completely slowed down.
Maybe you’ve told your doctors about these symptoms, but they will never tell you that this is a warning sign of mitochondrial dysfunction, because keeping you dependent on prescriptions and symptom management makes them billions of dollars.
And when I tell them there’s one single molecule with over 150 years of medical use, something that can restore mitochondrial function by rescuing failing cellular respiration and reigniting their metabolic rate at the cellular level, they look at me like I’m crazy.
But three weeks later, they always come back in tears, thanking me because they feel like a new person.
Their energy returns, the brain fog lifts, their body temperature normalizes, they’re thinking clearer, feeling warmer, their metabolism kicks back into gear, and they’re performing at a level they haven’t experienced since their twenties.
This molecule is called Methylene Blue.
And every time I mention it, I get the look.
Wide eyes. Raised eyebrows.
That “Isn’t methylene blue just another overhyped fad?” face.
And honestly? I get it.
It sounds sketchy.
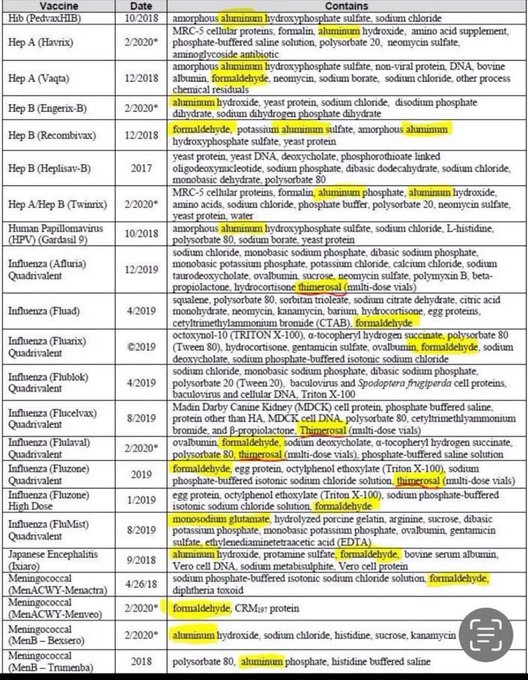
But when you’re choosing a methylene blue supplement, you need to make sure it works and doesn’t damage your thyroid. Most people think purity is all that matters, but they’re missing the hidden danger.
When you give your body methylene blue that’s verified pharmaceutical-grade, something remarkable happens.
Your mitochondria wake back up.
They start producing ATP efficiently again.
They repair cellular respiration.
Your metabolism reignites at the cellular level.
They even begin functioning like they did when you were younger.
I’ve taken it myself, every day for over 8 years.
And I recommend it to nearly every patient I work with who struggles with slow metabolism, brain fog, or low energy.
Why?
Because when you get ACTIVE methylene blue, it’s the one compound that mitochondrial researchers have proven acts as an alternative electron carrier in the electron transport chain, bypassing damaged complexes and restoring cellular ATP production—the fundamental currency of metabolism itself.
It helps replace multiple expensive metabolism boosters and nootropics by fixing the root cellular problem your body has been suffering from.
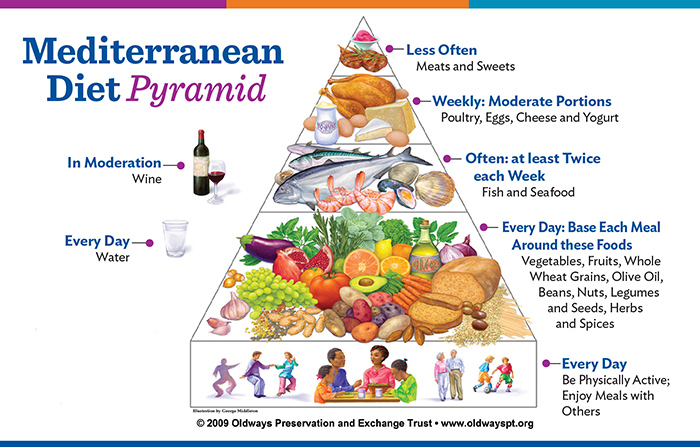
Just 5 drops a day could help you:
Replace 3-5 different metabolism and cognitive supplements with one solution.
Wake up with natural energy instead of exhaustion and sluggishness.
Stop the cycle of caffeine dependence and afternoon crashes.
Experience sustained metabolism without the jitters or tolerance buildup.
Clear the brain fog that’s been holding you back.
Feel warm and energized without constant fatigue.
Think faster and process information more efficiently.
Experience genuine metabolic vitality you haven’t had in years.
Save thousands of dollars every year on expensive supplement stacks.
It’s backed by over 150 years of medical use. It’s scientifically validated. And when done right, it works.
No prescriptions. No dependency. Just real support for your mitochondria’s natural energy production and metabolic function.
I take it every morning. And now… so do the patients I work with who refuse to accept metabolic decline and chronic fatigue.
It’s become my daily insurance policy. Five drops. Pure energy. Repeat.
If you read the thousands of reviews, you’ll see people breaking free from slow metabolism and brain fog.
This little bottle changed their relationship with energy and metabolic performance, and it could change yours too.